In recent years, TIM-3 and Alzheimer’s disease have emerged as critical focal points in the quest to understand and combat neurodegenerative diseases. Research led by experts like Vijay Kuchroo has uncovered the potential of TIM-3 as a checkpoint molecule that inhibits the activity of microglia, the brain’s immune cells. These findings suggest that by blocking TIM-3, we can enhance the microglia’s ability to clear amyloid plaques associated with Alzheimer’s, leading to improvements in cognitive function. Such innovative approaches represent a promising direction in Alzheimer’s research, merging insights from immune system therapy with neurology. As studies continue to explore the implications of TIM-3 in cognitive improvement, we may inch closer to effective therapies for this devastating condition.
The investigation into the connection between the TIM-3 molecule and Alzheimer’s disease highlights a groundbreaking approach to tackling memory impairment linked to aging. By exploring immune response mechanisms, researchers are identifying ways to enhance microglia function, potentially revolutionizing the treatment landscape for dementia and related disorders. Instead of solely addressing amyloid plaques, this new strategy focuses on the regulation of immune checkpoints, leading to significant changes in how we perceive and treat neurodegenerative ailments. With ongoing cognitive improvement studies leveraging immune system pathways, the future of Alzheimer’s treatment may lie in the intersection of immunology and neurology.
Understanding TIM-3’s Role in Alzheimer’s Disease
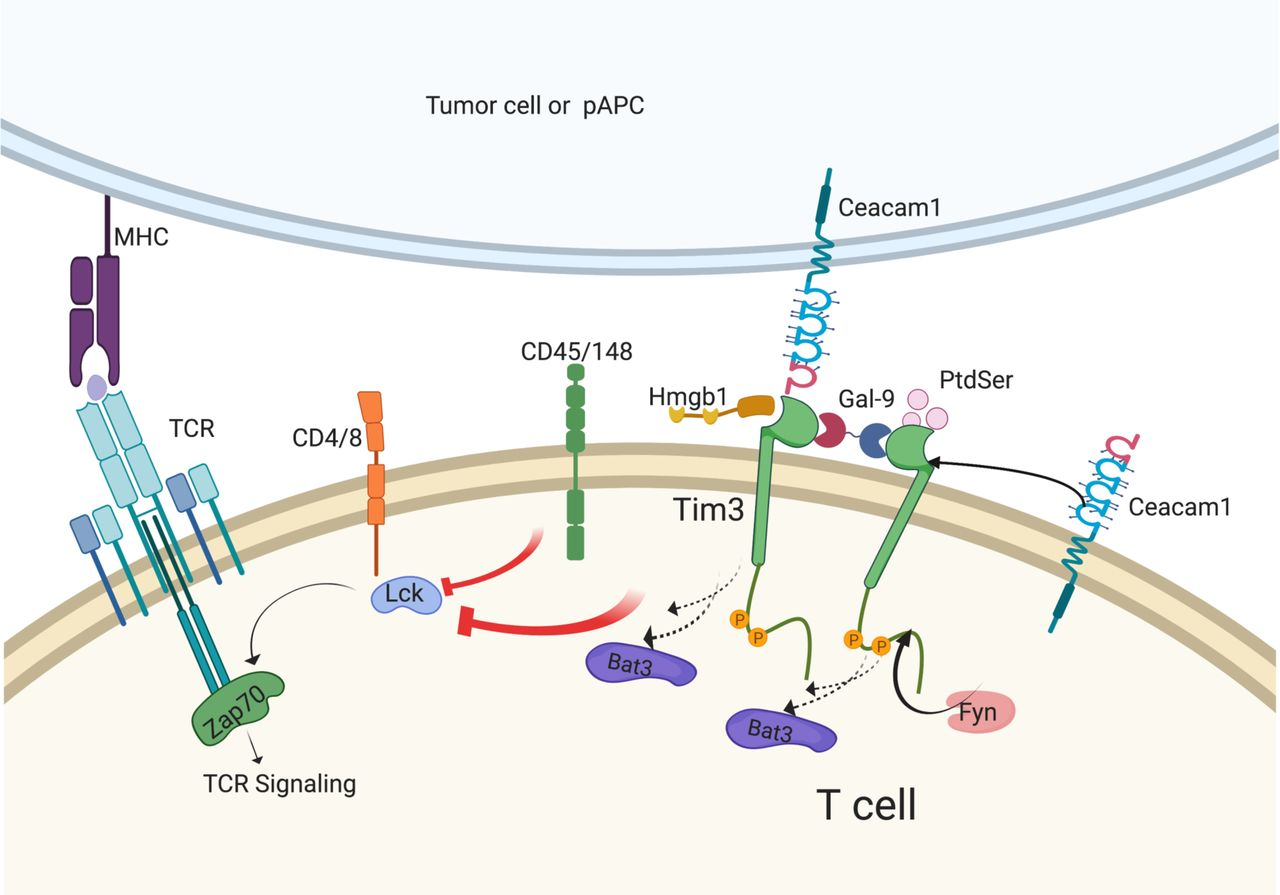
TIM-3 is a critical checkpoint molecule that plays an inhibitory role in the immune response, and its involvement in Alzheimer’s disease (AD) has garnered significant attention in recent research. Recent studies indicate that TIM-3 expression on microglia, the brain’s resident immune cells, can interfere with their ability to clear amyloid-beta plaques, which are characteristic of Alzheimer’s pathology. This dysfunction is particularly prevalent in late-onset Alzheimer’s, where elevated TIM-3 levels may correlate with worsened cognitive outcomes. Effective strategies targeting TIM-3 could unlock new avenues for therapeutic interventions that address the biological underpinnings of AD.
By deleting the TIM-3 gene in experimental models, researchers have demonstrated a marked improvement in microglial function, enabling these immune cells to resume their role in plaque clearance. This suggests that TIM-3 not only acts as a barrier to immune functionality during Alzheimer’s progression but also signifies its potential as a therapeutic target. Ongoing research aims to evaluate whether anti-TIM-3 antibodies can reverse cognitive decline in Alzheimer’s models, highlighting a promising path forward in the long quest for effective Alzheimer’s treatments.
Microglia: The Immune Warriors of the Brain
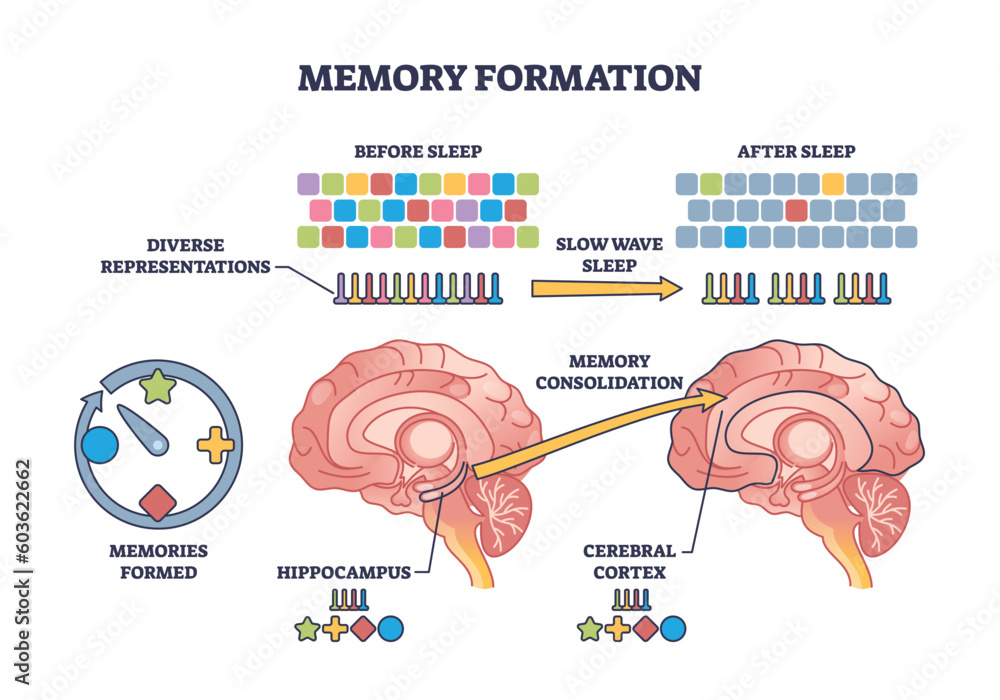
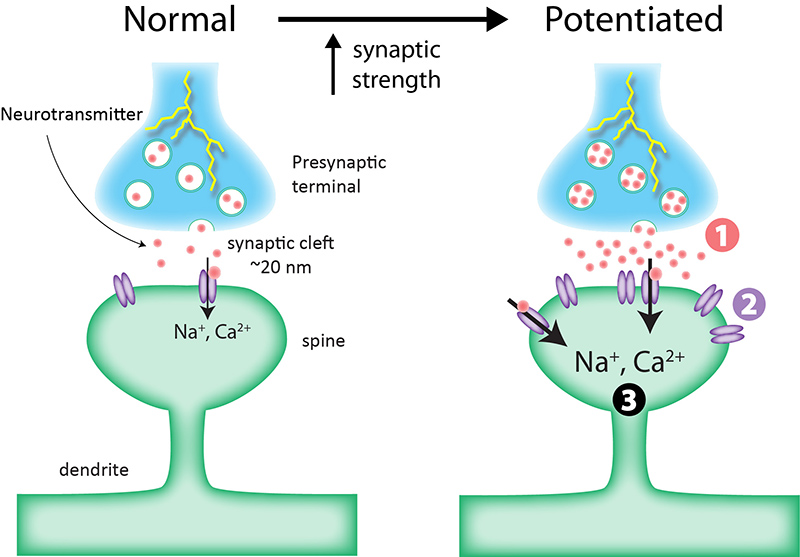
Microglia serve as the primary immune defense in the central nervous system, undertaking essential roles in both brain health and disease. Under normal conditions, microglia actively participate in synaptic pruning, a process crucial for memory formation and clearing out unnecessary cellular debris. However, their function changes with aging and in the presence of neurodegenerative diseases such as Alzheimer’s. The increased expression of TIM-3 inhibits microglial phagocytic activity, preventing these immune cells from effectively tackling amyloid plaques, thereby exacerbating cognitive decline.
As microglia adopt a homeostatic state influenced by TIM-3 signaling, they lose their ability to respond effectively to pathological changes. This underscores the importance of maintaining microglial health for cognitive longevity and highlights the potential benefits of therapies aimed at modulating TIM-3 activity. Understanding microglial function in the context of signaling pathways like TIM-3 can help develop targeted immune system therapies that may rejuvenate microglia and improve cognitive functions in Alzheimer’s patients.
Innovative Therapeutic Strategies Against Alzheimer’s
Recent developments suggest that repurposing immune strategies used in cancer therapy could pave the way for breakthroughs in Alzheimer’s treatment. For example, anti-TIM-3 antibodies, which showed promise in oncology by reinvigorating T cell function, might similarly enhance microglial activity in Alzheimer’s. This innovative thinking aligns with the broader goal in Alzheimer’s research to find immune-based therapies that effectively manage neuroinflammation and promote cognitive improvement, potentially offering better outcomes than traditional approaches.
The potential of TIM-3 inhibitors is substantiated by findings that demonstrate enhanced microglial clearance of amyloid plaques upon TIM-3 deletion. This emerging therapeutic landscape invites further exploration into the safety and efficacy of anti-TIM-3 treatments in clinical settings. As Alzheimer’s research progresses, leveraging insights from immune system therapy will be pivotal in developing comprehensive treatment plans that restore brain health and improve cognitive function for those affected by neurodegenerative diseases.
Cognitive Improvement Studies in Alzheimer’s Trials
Cognitive improvement studies are essential for evaluating the effectiveness of new Alzheimer’s treatments, particularly those targeting immune systems and related biomarkers like TIM-3. These studies typically involve assessing the ability of treatment candidates to enhance memory functions or reduce behavioral symptoms in animal models. The challenge lies in translating these findings to human trials, which requires careful design and positive outcomes from preliminary studies involving animal subjects, especially those genetically engineered to reflect human-like disease characteristics.
Recent advancements have shown promising results in cognitive behavior tests among mice lacking TIM-3, reinforcing the impact of this immune checkpoint on memory performance. These preclinical findings encourage the design of human clinical trials that will assess TIM-3 antagonists’ capability to provide cognitive benefits in Alzheimer’s patients. Successful results in these trials could redefine treatment paradigms, offering hope for more effective interventions against the cognitive decline associated with Alzheimer’s disease.
The Interaction Between Alzheimer’s Disease and the Immune System
The interaction between Alzheimer’s disease and the immune system is a growing area of focus in understanding the disease’s complexities. Traditionally viewed as a neurodegenerative condition primarily affecting neuronal function, recent insights highlight that immune dysregulation also plays a crucial role in the pathology of Alzheimer’s. The expression of TIM-3 on microglia is a prime example, revealing how immune checkpoints can inhibit the clearance of neurotoxic substances, making it a critical factor in the development and progression of Alzheimer’s.
Anomalies in immune responses due to factors such as gene polymorphisms can exacerbate the accumulation of harmful substances, leading to further neuronal damage. As researchers continue to unravel these intricate connections, the potential for developing immune-based therapies increases. Understanding how to modulate the immune response—specifically through checkpoint molecule inhibition like TIM-3—could be essential for advancing treatment approaches that address both cognitive impairment and plaque pathology in Alzheimer’s disease.
Exploring Genetic Risk Factors in Alzheimer’s Disease
Genetic risk factors for Alzheimer’s disease, including polymorphisms in the TIM-3 gene, play an integral role in an individual’s susceptibility to the illness. Studies have shown that certain variations in the HAVCR2 gene, which encodes TIM-3, are associated with increased risk of developing late-onset Alzheimer’s. Such genetic insights are valuable for understanding individual differences in disease progression and response to treatment, ultimately aiding in the development of more tailored therapeutic strategies that address these specific risk profiles.
Incorporating genetic profiles into clinical studies can enhance our comprehension of how variations in immune checkpoint molecules, like TIM-3, affect Alzheimer’s pathology. By identifying individuals at higher risk based on their genetic makeup, researchers can prioritize them in clinical trials for immune therapies. This precision medicine approach emphasizes the need for genetics-informed strategies in Alzheimer’s research, leading to more nuanced understanding and treatment of this complex neurodegenerative disorder.
The Significance of Amyloid Plaques in Alzheimer’s Disease
Amyloid plaques are hallmark features of Alzheimer’s disease, critical for understanding its progression and biological basis. The presence of these plaques, primarily composed of aggregated beta-amyloid peptides, triggers neuroinflammation and contributes to neuronal dysfunction. Their accumulation is directly linked to cognitive decline, as they interfere with synaptic function and promote microglial activation, leading to chronic inflammatory responses that further exacerbate brain damage.
The role of TIM-3 in mediating the response to amyloid plaques presents an exciting avenue for research. As TIM-3 inhibits microglial activity, the accumulation of plaques continues unchecked, resulting in severe cognitive impairment in patients. By targeting TIM-3 and restoring microglial function, researchers hope to enhance the clearance of amyloid plaques, providing a potential therapeutic strategy that not only alleviates plaque burden but also enhances cognition in Alzheimer’s patients.
Collaboration in Alzheimer’s Research: The Key to Innovation
Collaboration stands at the forefront of effective Alzheimer’s research, integrating diverse expertise from neurology, immunology, genetics, and pharmacology. Innovative studies like the one investigating TIM-3 showcase the power of interdisciplinary approaches, blending insights from cancer therapy with neurodegenerative disease treatment. Collaborators from institutes such as Harvard Medical School and Brigham and Women’s Hospital are vital in advancing research endeavors that harness shared knowledge and resources, driving forward our understanding of Alzheimer’s.
These collaborative efforts facilitate not only the pooling of research expertise but also the development of comprehensive treatment modalities that address multiple facets of the disease. As scientists work together to decode the intricate mechanisms behind Alzheimer’s, combining their findings with innovative therapeutic approaches could lead to breakthroughs that change the landscape of Alzheimer’s care, ultimately improving the quality of life for millions impacted by this devastating disease.
Future Directions in Alzheimer’s Therapeutics: The Role of TIM-3
The future of Alzheimer’s therapeutics may hinge significantly on the role of TIM-3 as a modulator of immune response within the brain. With ongoing research focusing on therapies that inhibit TIM-3 signaling, the potential to rejuvenate microglial function opens up exciting possibilities for addressing one of the disease’s fundamental pathological features—the accumulation of amyloid plaques. By unlocking the immunological barriers established by TIM-3, scientists aim to develop treatments that restore homeostasis in the brain, further aiming to halt cognitive decline.
As researchers push the boundaries of current knowledge, antibody-based therapies targeting TIM-3 may soon transition from the bench to clinical trials, promising new hope for Alzheimer’s patients. The burgeoning field of immunotherapy offers an optimistic view for future treatment options, where immune modulation can drastically alter the trajectory of Alzheimer’s disease and fundamentally improve cognitive outcomes for affected individuals.
Frequently Asked Questions
What is TIM-3 and how is it related to Alzheimer’s disease?
TIM-3 (T-cell immunoglobulin and mucin domain-containing protein 3) is an immune checkpoint molecule linked to late-onset Alzheimer’s disease (AD). It plays a crucial role in regulating immune reactions in the brain, particularly inhibiting microglia, the brain’s immune cells, from clearing amyloid plaques that accumulate in Alzheimer’s patients, thus contributing to cognitive decline.
How do TIM-3 and microglia function together in the context of Alzheimer’s research?
In Alzheimer’s disease, microglia express high levels of TIM-3, which prevents them from effectively clearing harmful amyloid plaques. This inhibitory mechanism is critical as it hampers the microglial function needed to manage neurodegenerative diseases, making it a focus of Alzheimer’s research aiming to restore normal microglia activity and improve cognitive functions.
Can blocking TIM-3 enhance memory functions in Alzheimer’s disease models?
Yes, studies have shown that deleting or blocking TIM-3 in animal models leads to enhanced microglial activity, which helps clear amyloid plaques. This intervention has demonstrated improvements in memory function, highlighting the therapeutic potential of TIM-3 blockade in combating cognitive decline associated with Alzheimer’s disease.
What therapeutic approaches are being explored involving TIM-3 for Alzheimer’s disease?
Various therapeutic strategies targeting TIM-3 include the use of anti-TIM-3 antibodies or small molecules to inhibit its function. These therapies aim to reactivate microglia, enabling them to perform their role in plaque clearance and potentially reversing some cognitive impairments seen in Alzheimer’s disease.
How significant are the findings related to TIM-3 and Alzheimer’s in recent studies?
Recent studies have indicated that the role of TIM-3 as an inhibitor of microglial function is significant in Alzheimer’s research. By understanding how TIM-3 affects plaque clearance and memory, researchers hope to develop effective immune system therapies that could change the course of Alzheimer’s disease.
What are the implications of TIM-3 gene polymorphisms in Alzheimer’s disease?
Polymorphisms in the TIM-3 gene (HAVCR2) have been associated with an increased risk for Alzheimer’s disease. Affected individuals often exhibit higher expression levels of TIM-3 in microglia, which can hinder plaque removal and exacerbate cognitive issues, making genetic variations in TIM-3 a focal point for understanding susceptibility to Alzheimer’s.
What does TIM-3 blockade mean for future Alzheimer’s therapies?
Blockade of TIM-3 may pave the way for novel Alzheimer’s therapies that enhance microglial functions, potentially rescuing cognitive abilities in affected individuals. Given the challenges faced with existing Alzheimer’s drugs, TIM-3 represents a promising target for developing innovative treatment strategies.
What role does the immune system play in Alzheimer’s disease, specifically concerning TIM-3?
The immune system, particularly through the action of TIM-3, plays a dual role in Alzheimer’s disease. While it attempts to regulate brain inflammation and clear amyloid plaques through microglial activity, overexpression of TIM-3 can lead to dysfunction and impaired plaque clearance, contributing to neurodegenerative processes.
How does TIM-3 relate to cognitive improvement studies in Alzheimer’s disease research?
Cognitive improvement studies in Alzheimer’s research often focus on the modulation of immune responses, including TIM-3 regulation. By targeting TIM-3, researchers aim to enhance the ability of microglia to clear amyloid plaques, thereby potentially improving cognitive functions and alleviating symptoms of Alzheimer’s disease.
What is the ultimate goal of TIM-3 research in relation to Alzheimer’s disease treatment?
The ultimate goal of TIM-3 research in Alzheimer’s disease is to develop therapies that can effectively block or modify TIM-3’s inhibitory effects on microglia, thus facilitating plaque clearance, improving cognitive functioning, and providing a new avenue for treating Alzheimer’s patients.
| Key Points | Details |
|---|---|
| TIM-3 and Alzheimer’s Disease | The study investigates the role of the TIM-3 molecule in the context of Alzheimer’s disease, showing its potential as a target for treatment. |
| Mechanism of TIM-3 | TIM-3 acts as a checkpoint molecule that inhibits microglia, preventing them from clearing amyloid plaques in the brain. |
| Research Findings | In mice lacking TIM-3, microglia were able to clear amyloid plaques, leading to improved memory and cognitive function. |
| Clinical Implications | Anti-TIM-3 therapies may offer a new approach for Alzheimer’s treatment, potentially allowing existing cancer therapies to be repurposed. |
| Future Directions | Ongoing research aims to test the efficacy of human anti-TIM-3 antibodies in mouse models of Alzheimer’s disease. |
Summary
TIM-3 and Alzheimer’s disease are at the forefront of promising research that seeks to leverage immune system strategies to combat neurodegeneration. This study highlights TIM-3 as a crucial checkpoint molecule that, when inhibited, allows brain immune cells to effectively clear harmful plaques, potentially restoring cognitive function. The innovative approach of utilizing anti-TIM-3 therapies may pave the way for novel treatments in Alzheimer’s, offering hope for millions affected by this disease.