Neurodegenerative disease research plays a critical role in understanding and combating conditions like Alzheimer’s disease, which affects millions globally. As scientists delve into the complexities of neurobiology, breakthrough discoveries highlight the significance of microglial cells, the immune defenders of the brain, in maintaining brain health. These cells are not just passive observers; they actively participate in clearing out damaged neurons and sculpting neural circuits. Recent studies illustrate how improper functioning of these microglial cells can lead to devastating disorders, including Alzheimer’s and Huntington’s disease. Through such revelations, researchers are paving the way for innovative biomarkers and treatments that could change the lives of those impacted by neurodegenerative diseases.
Research in the field of neurodegenerative disorders encompasses the exploration of conditions that lead to the gradual degeneration of neurons, such as Alzheimer’s and Parkinson’s disease. Scientists are increasingly focusing on the role of the brain’s immune cells, known as microglia, to unravel their complex interactions and effects on neural health. By examining the pathways these unique cells take in response to injury or disease, researchers hope to uncover new insights and therapeutic approaches. Among the recent advancements in neuroscience discoveries is the understanding of aberrant synaptic pruning, a process that, when disrupted, may contribute to severe cognitive decline. This multifaceted approach not only sheds light on the underlying mechanisms of brain health but also fosters the development of targeted interventions for those affected by these debilitating conditions.
Understanding Neurodegenerative Disease Research: Microglial Cells’ Role
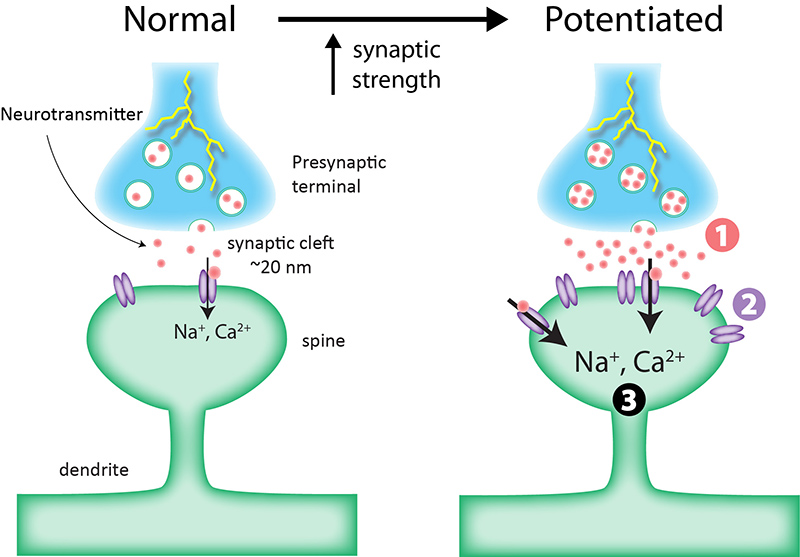
Neurodegenerative disease research has gained significant traction over the past few decades, particularly regarding the role of microglial cells in brain health. These immune cells are essential for maintaining the delicate balance of synaptic pruning, which is crucial for proper neural network function. However, as Beth Stevens’ groundbreaking research indicates, mismanagement or aberrant pruning by microglia can lead to devastating conditions such as Alzheimer’s disease and Huntington’s disease. Understanding this process not only sheds light on the pathophysiology of these disorders but also opens up new avenues for potential therapeutic interventions.
In the realm of neurobiology, recognizing microglial cells as both protectors and potential aggressors in the brain is a significant shift in how we approach neurodegenerative diseases. Stevens and her team at the Broad Institute have explored how these cells respond to neuronal damage or inflammation. Their pioneering work has laid the groundwork for identifying new biomarkers that could lead to early detection and diagnosis of conditions like Alzheimer’s. As we delve deeper into neurobiology and neuroscience discoveries, the role of microglia emerges as a crucial element in developing targeted treatments for these insidious diseases.
The Impact of Basic Science on Neuroscience Discoveries
The journey of scientific discovery often begins with basic research, an essential component that can lead to unforeseen advancements in treating complex diseases. Beth Stevens exemplifies this through her exploration of microglial cell function, which stemmed from fundamental scientific inquiries into neurobiology. Initially perceived as unrelated to human conditions, her research provided substantial insights that bridged the gap between basic science and practical applications in neurodegenerative disease research. This demonstrates the critical importance of curiosity-driven investigations in unveiling the underlying mechanisms of brain health.
Stevens’ work underscores a vital lesson in the field of neuroscience: breakthroughs do not always materialize immediately, and they often necessitate a long-term commitment to research. The support from federal agencies like the National Institutes of Health fuels this endeavor, allowing scientists to explore intricate biological questions. As the Stevens Lab’s findings continue to proliferate, they not only enhance our understanding of brain health but also pave the way for innovative strategies in combating Alzheimer’s disease and related disorders through advanced therapeutic approaches.
Innovations in Biomarkers for Early Detection of Alzheimer’s
The quest for effective biomarkers for Alzheimer’s disease is an exciting frontier in neurodegenerative disease research. With the rising prevalence of Alzheimer’s among older populations, identifying reliable biomarkers is imperative for early diagnosis and intervention. Recent studies led by Beth Stevens indicate that alterations in microglial cell behavior could serve as potential indicators of Alzheimer’s pathology in the brain. By detecting these changes at an early stage, it may become possible to implement preventative strategies or targeted therapies to halt disease progression.
Advancements in neuroscience provide novel methodologies to examine the immune responses of the brain, particularly focusing on microglial activity. Stevens’ research sheds light on how these cells respond to various stimuli associated with neuronal injury and inflammation. By harnessing this knowledge, researchers are developing new techniques that could lead to the identification of specific biomarkers indicative of Alzheimer’s. As we continue to unravel the complexities of neurobiology, these innovations hold immense promise for improving the management and treatment of Alzheimer’s disease.
Exploring Synaptic Pruning and Its Implications for Brain Health
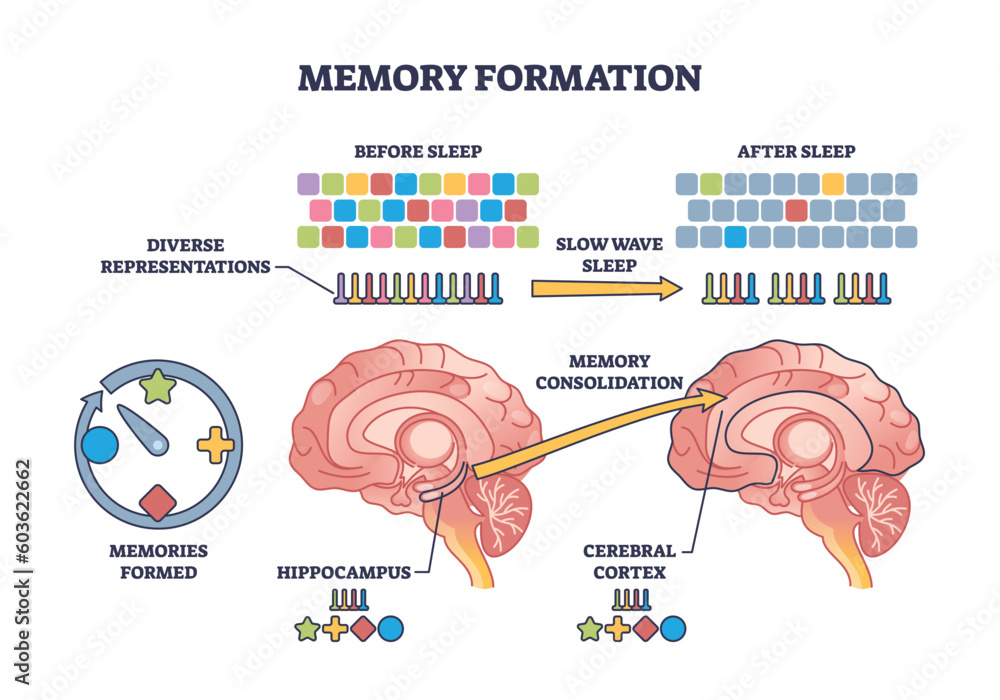
Synaptic pruning is a fundamental process by which the brain refines its neural connections, crucial for optimal brain function. In healthy development, this process allows the brain to adapt and reorganize. However, when microglial cells mismanage pruning, it can contribute to neurodegenerative diseases like Alzheimer’s. Beth Stevens’ research emphasizes the delicate interplay between microglia and synapses, illustrating how disruptions in this balance can lead to cognitive decline. Gaining insights into synaptic pruning can unravel the complexities of brain health and inform strategies to mitigate risks of neurodegeneration.
Understanding the dynamics of synaptic pruning not only enhances our grasp of normal brain function but also illuminates the pathological processes involved in neurological disorders. Researchers are now investigating how modulating microglial activity could restore balance in synaptic pruning, thus offering therapeutic potential for conditions like Alzheimer’s. As neuroscience continues to evolve, the exploration of these mechanisms will undoubtedly shape future approaches to preserving brain health and addressing the challenges posed by neurodegenerative diseases.
Federal Support in Advancing Neuroscience Research
Federal funding, particularly from the National Institutes of Health, plays a pivotal role in propelling neuroscience research forward. This support is crucial for scientists like Beth Stevens, enabling them to pursue innovative lines of inquiry into neurodegenerative diseases such as Alzheimer’s. The significant financial backing allows for exploration of novel concepts, including the role of microglial cells in synaptic pruning and neuronal health. As foundational research flourishes with adequate support, it lays the groundwork for transformative discoveries that can ultimately revolutionize treatment protocols.
Such investments in basic science underscore the importance of a sustained commitment to exploring the unknown in neurobiology. The work conducted in labs like Stevens’ not only contributes to a deeper understanding of disease mechanisms but also creates a scholarly ecosystem where findings can lead to real-world applications. With ongoing federal support, the neuroscience community is better equipped to tackle the complexities of neurodegenerative diseases, striving to improve patient outcomes and advance public health initiatives.
Transformative Discoveries in Alzheimer’s Disease Mechanisms
Discoveries in neurobiology often pave the way for transformative breakthroughs in understanding Alzheimer’s disease mechanisms. Beth Stevens’ research on microglial cells has unveiled the dual roles they play in maintaining brain health and their potential contribution to neurodegeneration. By investigating the processes of synaptic pruning and microglial activation, scientists are gaining crucial insights into the pathways that lead to the development of Alzheimer’s. Such findings are not just academic; they yield practical implications for developing therapies that can alter the disease course.
Recent neuroscience discoveries have opened new avenues for therapeutic intervention in Alzheimer’s disease, driven by the understanding of how microglial cells impact synaptic health. By targeting these immune cells with new drugs or therapies, researchers hope to restore normal pruning processes and protect against cognitive decline. The implications of these transformative discoveries are profound, as they hold promise for not only enhancing our understanding of Alzheimer’s but also providing novel treatment avenues that could significantly improve the lives of millions.
The Future of Neurobiology in Treating Alzheimer’s Disease
The future of neurobiology holds immense potential for addressing the challenges presented by Alzheimer’s disease. As research progresses, the integration of findings from numerous studies into microglial function and synaptic pruning will likely lead to innovative treatment modalities. With scholars like Beth Stevens at the forefront, we are beginning to see a shift towards developing approaches that are more targeted and personalized. The opportunity to tailor treatments based on an individual’s specific neurobiological profile marks a significant advancement in the fight against Alzheimer’s.
Moreover, the collaboration among neuroscience researchers, clinicians, and regulatory bodies will be essential in translating these discoveries into clinical practices. The continuous engagement with cutting-edge neurobiology research will inform public health policy and lead to more effective strategies for managing Alzheimer’s disease. As we look forward to future breakthroughs, the commitment to understanding the complexities of brain health and neurodegenerative diseases will undoubtedly shape the landscape of treatment options available for patients.
Placing Emphasis on Curiosity-Driven Research
Curiosity-driven research remains a cornerstone of scientific innovation in neurodegenerative disease studies. The work of Beth Stevens illustrates how following scientific curiosity can lead to unexpected discoveries with profound implications for brain health. Such research emphasizes the importance of allowing scientists to explore avenues without immediate expectations for direct applications. This approach fosters an environment that generates new ideas and questions, ultimately contributing to the body of knowledge around diseases like Alzheimer’s.
Encouraging curiosity in scientific inquiry can unlock new paradigms in understanding neurodegenerative diseases. As researchers investigate fundamental biological processes, unexpected correlations often emerge, paving the way for novel therapeutic strategies. In fostering a culture of inquiry, the neuroscience field stands to benefit significantly, enhancing efforts toward breakthrough discoveries that could transform the lives of those affected by conditions like Alzheimer’s disease. The potential impact of such research extends beyond academia, influencing clinical practices and enhancing public health initiatives.
Navigating the Challenges in Neurodegenerative Disease Research
Neurodegenerative disease research faces several challenges that necessitate a multifaceted approach. Considerations such as the complexity of brain pathology, ethical implications, and the need for longitudinal studies complicate our understanding of conditions like Alzheimer’s disease. However, as noted by Beth Stevens, embracing these challenges can lead to greater discoveries. The evolving understanding of microglial cells and their roles in neurodegeneration highlights the necessity to adapt research methodologies to address emerging questions and hypotheses.
Collaboration within the scientific community and with external stakeholders is paramount in navigating these challenges effectively. By pooling resources and integrating diverse perspectives, researchers can enhance the research landscape for neurodegenerative diseases. Building interdisciplinary teams that include neuroscientists, clinicians, and geneticists can drive innovation and foster dynamic discussions around complex issues. As we face the pressing reality of an aging population, addressing these challenges with creativity and persistence remains crucial in advancing neurodegenerative disease research.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells are crucial in Alzheimer’s disease research as they act as the brain’s immune system. They monitor brain health by clearing dead neurons and pruning synapses, which is vital for maintaining neural connectivity. Aberrant microglial activity can contribute to neuroinflammation and synaptic loss, leading to the progression of Alzheimer’s disease and other neurodegenerative disorders.
How does neurobiology influence the understanding of neurodegenerative diseases?
Neurobiology plays a fundamental role in understanding neurodegenerative diseases by elucidating the cellular mechanisms and pathways involved in brain health. Research in neurobiology helps uncover how processes like synaptic pruning by microglial cells can contribute to conditions such as Alzheimer’s disease, allowing for the identification of potential biomarkers and therapeutic targets.
What recent neuroscientific discoveries have impacted Alzheimer’s disease treatment strategies?
Recent neuroscientific discoveries have significantly impacted Alzheimer’s disease treatment strategies, particularly findings related to the function of microglial cells. Understanding how these immune cells contribute to synaptic pruning has opened new avenues for developing treatments that could modify the disease progression and enhance cognitive function in patients.
Why is basic science essential for advances in neurodegenerative disease research?
Basic science is essential for advances in neurodegenerative disease research as it lays the groundwork for understanding complex biological processes. For example, explorations into microglial cell functions and their role in synaptic health provide insights that are critical for developing targeted therapies for diseases like Alzheimer’s.
How does federal funding support neurodegenerative disease research initiatives?
Federal funding plays a vital role in supporting neurodegenerative disease research initiatives by providing resources for groundbreaking studies. This funding allows researchers, like those at the Stevens Lab, to explore fundamental aspects of diseases such as Alzheimer’s, which can lead to innovative treatments and improve patient outcomes.
What are biomarkers and how are they relevant to neurodegenerative disease research?
Biomarkers are biological indicators that can signal the presence or progression of neurodegenerative diseases like Alzheimer’s. In neurodegenerative disease research, identifying specific biomarkers associated with microglial dysfunction or synaptic alteration can aid in early diagnosis and treatment monitoring, leading to better management of the disease.
How does understanding synaptic pruning contribute to advancements in neuroscience?
Understanding synaptic pruning is crucial for advancements in neuroscience as it reveals the underlying mechanisms of brain health and degeneration. Research showing how microglial cells regulate synaptic pruning provides insights into neurodevelopmental and neurodegenerative conditions, facilitating the development of targeted therapies to mitigate cognitive decline in diseases like Alzheimer’s.
What is the significance of Beth Stevens’ research at Boston Children’s Hospital?
Beth Stevens’ research at Boston Children’s Hospital is significant as it has transformed our understanding of the immune functions of microglial cells in the brain, revealing their role in conditions like Alzheimer’s disease. Her findings have laid the foundation for the development of new biomarkers and treatment strategies that could greatly impact care for millions affected by neurodegenerative diseases.
| Key Points | Details |
|---|---|
| Microglial Cells | Act as the brain’s immune system to clear out damaged cells and prune synapses. |
| Research Impact | Beth Stevens’ research is critical in understanding the role of microglial cells in neurodegenerative diseases like Alzheimer’s and Huntington’s. |
| New Discoveries | Aberrant pruning by microglia contributes to various neurodegenerative diseases, which can lead to new biomarkers and treatment options. |
| Funding Importance | Research heavily supported by NIH and federal grants, underscoring the necessity of federal funding in scientific advancements. |
| Curiosity-Driven Science | Basic science has led to unexpected pathways to address human diseases and conditions. |
Summary
Neurodegenerative disease research is increasingly focusing on the role of microglial cells in brain health, as demonstrated by Beth Stevens’ work at Boston Children’s Hospital. Her findings highlight how these immune cells are crucial for maintaining neuronal integrity but can also contribute to diseases like Alzheimer’s when their function goes awry. With federal support paving the way, Stevens’ innovative discoveries provide a foundation for developing new treatments, showcasing the essential link between basic science and potential clinical applications.