Brain cancer prediction, particularly in pediatric populations, represents a significant advancement in medical science, leveraging innovative technologies such as AI and machine learning. Recent research at Mass General Brigham showcased how an AI tool analyzing MRI scans can more accurately assess the risk of glioma relapse compared to traditional screening methods. This tool’s ability to predict recurrence is crucial, as pediatric brain tumors are often treatable but can pose severe risks if they return. By optimizing the process of monitoring pediatric oncology patients, we can reduce the emotional burden on families and improve the overall care pathway. As healthcare evolves, integrating machine learning into diagnostics offers hope for better management of pediatric brain tumors and enhanced patient outcomes.
The forecast of brain cancer, especially among younger patients, is transforming with the incorporation of advanced technologies like artificial intelligence and predictive analytics. Groundbreaking studies have illustrated the effectiveness of AI in identifying the likelihood of glioma reoccurrence, far surpassing conventional methodologies. Such predictive insights are essential for tailoring treatment approaches and minimizing the psychological toll on families dealing with pediatric cancer. By utilizing serial imaging techniques, notably MRI scans, healthcare professionals can harness this data to fine-tune treatment strategies and improve prognostic accuracy. In this dynamic landscape of pediatric oncology, the focus on early detection and personalized care is paramount for navigating the complexities associated with brain tumors.
Understanding Pediatric Brain Tumors
Pediatric brain tumors are a significant health concern, particularly because they often present unique challenges in diagnosis and treatment. Unlike adult brain tumors, the types found in children can vary greatly in terms of their biology, growth patterns, and responses to therapy. Common types include gliomas, medulloblastomas, and ependymomas, each requiring tailored treatment approaches. Early diagnosis is crucial, as it significantly impacts the treatment outcome and long-term survival rates for young patients.
The complexity of pediatric brain tumors lies not just in their variety but also in their location and association with neurological development. Tumors can affect areas of the brain responsible for critical functions such as motor skills, vision, and cognition, leading to a range of symptoms that can complicate diagnosis. Ongoing research into the genetic and molecular characteristics of these tumors is essential, as it paves the way for more effective therapies and potentially less invasive treatment options, benefiting the children’s quality of life.
The Role of AI in Pediatric Oncology
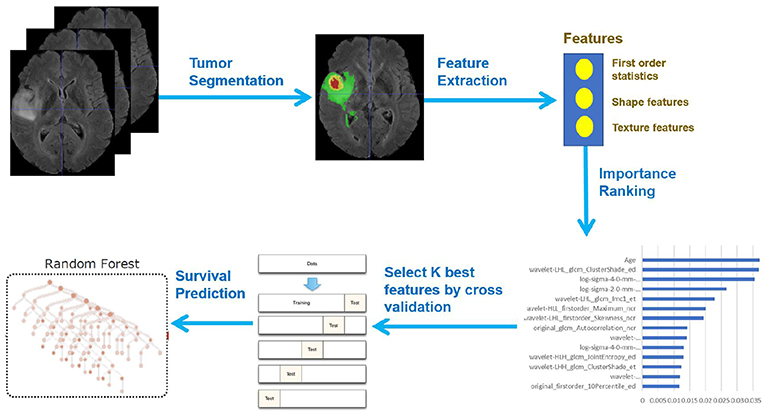
Artificial Intelligence (AI) is increasingly revolutionizing the field of pediatric oncology by enhancing the accuracy of predictions and treatment protocols. Utilizing sophisticated algorithms and machine learning techniques, AI can analyze vast datasets, including MRI scans, to identify patterns that human clinicians may overlook. This capability not only sharpens the focus on risk assessment but also tailors treatment plans based on individual patient profiles, improving overall care outcomes.
Moreover, AI’s application in pediatric oncology extends beyond diagnosis; it can predict treatment responses and monitor for potential relapse, especially in conditions like glioma. AI tools that utilize temporal learning are particularly promising, as they analyze serial images over time, providing deeper insights into tumor behavior and recurrence risks. This approach allows healthcare providers to allocate resources more effectively and develop proactive strategies for managing the health of young patients.
Machine Learning and Brain Cancer Prediction
Machine learning models play a pivotal role in brain cancer prediction, particularly in pediatric patients faced with gliomas. By leveraging advanced algorithms capable of processing extensive imaging data, these models can significantly outperform traditional methods in predicting relapse risk. A recent study highlighted that AI tools trained on multiple MRI scans could forecast recurrence with an accuracy rate of 75-89%, indicating a groundbreaking shift in how healthcare providers approach treatment and monitoring.
The integration of machine learning in healthcare, particularly for conditions as complex as pediatric brain tumors, marks a critical advancement towards personalized medicine. As more data becomes available, the ability of AI systems to learn from past cases enhances their predictive power and reliability. This not only improves patient care by identifying those who require more intensive monitoring or intervention but also reduces the stress and uncertainty experienced by families during follow-up treatments.
Leveraging MRI Scans for Enhanced Diagnosis
Magnetic Resonance Imaging (MRI) scans are a critical diagnostic tool in identifying brain tumors in children. They provide detailed images of the brain, allowing for accurate localization and characterization of tumors. The challenge, however, lies in differentiating benign conditions from malignant tumors and accurately assessing tumor progression over time. AI-assisted MRI analysis can improve the diagnostic accuracy by focusing on subtle changes across consecutive scans, thereby informing clinicians about the best course of action.
Incorporating machine learning algorithms into MRI analysis enables clinicians to harness large data sets effectively, enhancing the diagnostic process. This is particularly relevant in the context of gliomas, where understanding the tumor’s nature can significantly influence treatment decisions. With improved algorithms, clinicians can predict outcomes more accurately, which is essential for formulating individualized treatment plans that minimize adverse effects while maximizing therapeutic efficacy.
The Importance of Early Intervention in Glioma Treatment
Early intervention is crucial in the treatment of gliomas in pediatric patients, as it often leads to better outcomes. The ability to predict the risk of relapse before it occurs can significantly improve the management of these tumors. AI tools that analyze MRI scans sequentially provide insight into the patterns of tumor growth and potential recurrence, enabling clinicians to intervene earlier and personalize treatment strategies.
Furthermore, timely interventions can enhance the quality of life for young patients. By reducing the frequency of invasive procedures like MRI scans for low-risk patients, clinicians can alleviate the emotional and physical burden on families. This proactive approach ensures that high-risk patients receive necessary treatments sooner, ultimately contributing to improved survival rates and a better overall prognosis in pediatric oncology.
Challenges in Traditional Brain Cancer Monitoring
Traditional methods for monitoring brain cancer in children often involve frequent imaging, which can be both stressful and burdensome for young patients and their families. Long-term follow-up protocols commonly rely on single MRI scans, leading to a risk of misinterpretation of tumor activity and recurrence. This approach can create an anxious environment for patients who are uncertain about their treatment outcomes.
The need for a more refined strategy highlights the limitations of existing protocols. By integrating AI technologies that can interpret serial imaging data over time, healthcare providers can transition to a more patient-centric approach that minimizes unnecessary interventions, thereby enhancing the quality of life for patients. This shift towards smarter monitoring not only alleviates stress but also paves the way for more effective treatment plans in pediatric oncology.
Future Directions for Pediatric Oncology Research
As research continues to evolve in pediatric oncology, the integration of AI and machine learning into clinical practice is set to enhance the precision of brain cancer diagnosis and treatment. The results from studies utilizing AI to analyze brain scans illustrate a promising future where healthcare providers can significantly improve risk assessment for conditions like glioma. Ongoing collaboration between research institutions, clinicians, and technology developers will be crucial to translating these advancements into practical applications.
The future of pediatric oncology research also depends on inclusivity in data collection and the development of diverse datasets that reflect various demographics. Ensuring that research outcomes are applicable to different populations will strengthen the overall efficacy of AI-based tools. By focusing on these areas, researchers can drive forward innovative solutions that prioritize the health and well-being of children diagnosed with brain tumors.
Potential of Temporal Learning in Medical Imaging
Temporal learning represents a transformative approach in the realm of medical imaging, particularly in predicting glioma relapse. Unlike traditional methods that analyze single MRI scans, temporal learning utilizes a series of images taken over time to identify patterns indicative of tumor activity. This advanced technique allows algorithms to learn from the subtle changes that occur in a patient’s brain, ultimately leading to improved prediction accuracy.
The application of temporal learning in pediatric oncology has resulted in striking advancements, improving predictive accuracy from a mere chance level to a promising 75-89%. By enabling healthcare providers to discern high-risk patients effectively, this innovative method stands to change the landscape of follow-up and treatment protocols in pediatric brain cancer management.
Collaboration in Pediatric Brain Cancer Research
The fight against pediatric brain cancer like glioma demands a collaborative effort across various medical and research institutions. Partnerships among entities such as Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center exemplify the synergy needed to tackle the complexities of brain tumors in children. By pooling resources and expertise, these collaborations can accelerate research, enhance data collection, and ultimately improve patient care.
Such collaborative research initiatives play a crucial role in advancing clinical trials and validating findings that can lead to widespread changes in treatment guidelines. With a collective focus on utilizing AI and machine learning technologies, these partnerships not only drive innovation but also ensure that the latest advancements in diagnosis and treatment are available to the youngest patients facing brain cancer.
Frequently Asked Questions
What is the role of AI in predicting brain cancer in pediatric patients?
AI plays a significant role in predicting brain cancer, particularly in pediatric cases, by analyzing MRI scans over time to identify patterns that indicate relapse risk for conditions such as pediatric gliomas. This advanced machine learning technique enhances prediction accuracy compared to traditional one-scan approaches.
How do AI tools improve glioma relapse risk predictions compared to traditional methods?
AI tools improve glioma relapse risk predictions by utilizing temporal learning, where multiple MRI scans of a patient are analyzed chronologically. This method allows AI to detect subtle changes in brain imaging over time, leading to more accurate assessments of recurrence risk.
What advances in machine learning are being used for pediatric brain tumors?
Recent advances in machine learning, particularly those applied to healthcare, focus on using AI to analyze extensive datasets from multiple MRI scans of pediatric brain tumors. These methods enhance the ability to predict relapse in conditions like gliomas, offering more reliable outcomes for patient management.
What is the importance of MRI scans in the prediction of brain cancer recurrence?
MRI scans are essential in predicting brain cancer recurrence as they provide detailed imaging of the brain over time. The study demonstrates that by examining multiple scans with AI, clinicians can better assess the likelihood of glioma relapse, optimizing follow-up care.
Are AI-driven predictions beneficial for managing pediatric gliomas?
Yes, AI-driven predictions are beneficial for managing pediatric gliomas as they can accurately identify patients at risk of relapse. This allows for tailored follow-up care and treatment strategies, potentially reducing unnecessary stress from frequent imaging for low-risk patients.
How does temporal learning enhance the prediction of brain cancer relapse?
Temporal learning enhances the prediction of brain cancer relapse by training AI models to connect changes observed in consecutive MRI scans rather than relying on isolated images. This comprehensive analysis results in a better understanding of disease progression and relapse risk.
What are the potential clinical applications of AI in pediatric oncology?
Potential clinical applications of AI in pediatric oncology include improved risk stratification for brain cancer recurrence, optimizing surveillance strategies for patients, and guiding treatment decisions, especially in pediatric brain tumors like gliomas.
What are the next steps for AI research in brain cancer prediction?
The next steps for AI research in brain cancer prediction involve further validation of the temporal learning model across different clinical settings and launching clinical trials to determine its effectiveness in improving patient care and treatment outcomes.
| Key Point | Details |
|---|---|
| AI Tool Effectiveness | An AI tool significantly outperforms traditional methods in predicting relapse risk in pediatric glioma patients. |
| Study Context | Conducted by researchers from Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston, published in *The New England Journal of Medicine AI*. |
| Temporal Learning Methodology | AI uses temporal learning to analyze multiple MRI scans over time, improving the prediction of cancer recurrence. |
| Prediction Accuracy | Predictions of relapse risk achieved an accuracy of 75-89%, compared to about 50% for single image analysis. |
| Clinical Implications | Potential for reducing unnecessary MRIs for lower-risk patients and preemptively treating higher-risk patients with targeted therapies. |
| Future Directions | Further validation is needed before clinical application; future clinical trials expected to explore AI-informed care improvements. |
Summary
Brain cancer prediction is set to undergo a transformative shift with the advent of AI technologies that efficiently analyze multiple MRI scans over time. The recent study from Mass General Brigham demonstrates that this innovative approach can predict relapse risks in pediatric glioma patients with remarkable accuracy, significantly outperforming traditional methods. By employing temporal learning, the AI model synthesizes information from several scans, allowing for a more nuanced understanding of the disease’s progression. This advancement is a critical step towards enhancing patient care, offering hope for better treatment strategies and less invasive monitoring for children facing these challenging diagnoses.