Alzheimer’s research is at the forefront of understanding how neurodegenerative diseases like Alzheimer’s disease impact millions worldwide. Recent studies conducted by innovative neuroscientist Beth Stevens have illuminated the critical role of microglial cells, which serve as the brain’s immune system. These cells help maintain brain health by removing damaged cells and pruning synapses, an essential process for cognitive function. However, when microglial pruning goes awry, it can exacerbate conditions such as Alzheimer’s, leading to significant memory impairment. As the U.S. population ages, the advancements in Alzheimer’s treatment derived from this research hold promise for improving care and enhancing the quality of life for approximately 7 million affected Americans.
When discussing the fight against dementia, significant attention is directed towards innovative Alzheimer’s research, which is reshaping our understanding of cognitive decline in aging populations. This burgeoning field has revealed much about the role of brain health, particularly through the lens of neuroinflammation and the behavior of immune cells in the brain. Nobel-prize-winning scientists and researchers like Beth Stevens are leading the charge, focusing on the functions of specialized cells that protect our brain, such as microglia. Their work has opened up new avenues for addressing not only Alzheimer’s but also a range of neurodegenerative disorders. With continued investment in this pivotal research area, the future of Alzheimer’s therapy and early detection looks increasingly promising.
Understanding Microglial Cells: The Brain’s Immune System
Microglial cells serve a crucial role in the brain, acting as its immune defenders. These specialized cells constantly survey the nervous system for signs of dysfunction and damage, ensuring that the delicate balance of brain health is maintained. In recent years, research has illuminated their dual role in both protecting and potentially harming brain function, particularly in the context of neurodegenerative diseases. When microglia become activated due to injury or disease, they can either promote healing by removing cellular debris or contribute to inflammation, which can exacerbate conditions like Alzheimer’s disease.
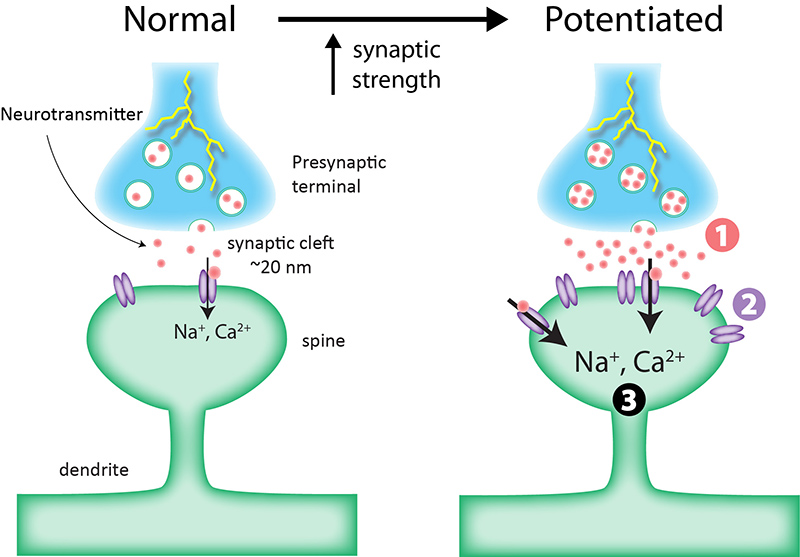
Beth Stevens, a leading figure in this field, emphasizes that understanding how microglial cells work offers profound implications for therapeutic strategies. Her groundbreaking research highlights how impaired microglial pruning processes can disrupt synaptic connectivity, leading to cognitive decline seen in Alzheimer’s patients. This insight opens doors for developing treatments that could enhance microglial function, potentially countering the progression of neurodegenerative disorders.
The Role of Alzheimer’s Research in Finding Effective Treatments
Alzheimer’s research is critical not just for understanding the disease’s complexities but also for paving the way for innovative treatments. As noted by Stevens, the connection between microglial activity and Alzheimer’s progression emphasizes the need for targeted therapies that address these underlying cellular mechanisms. The identification of biomarkers through ongoing research can facilitate earlier detection of the disease, allowing for timely intervention that can significantly improve patient outcomes.
Furthermore, with the expected doubling of Alzheimer’s cases in the coming decades, the stakes couldn’t be higher. Understanding how neuroinflammation, mediated by microglial cells, affects brain health is essential for developing new therapeutic strategies. Stevens’ collaborative work with institutions such as the Broad Institute illustrates how interdisciplinary approaches in Alzheimer’s research can lead to breakthroughs that ultimately enhance the quality of life for millions affected by this debilitating disease.
Innovative Discoveries in Neurodegenerative Disease Management
As the landscape of neurodegenerative disease research evolves, the discoveries made by scientists like Beth Stevens are paving the way for innovative management strategies. By elucidating the role of microglial cells in normal and pathological conditions, researchers are uncovering potential avenues for intervention that were previously unimaginable. For instance, Stevens’ findings suggest that manipulating microglial activity could provide a novel therapeutic angle for treating Alzheimer’s and similar disorders.
Moreover, these insights are crucial not only for understanding the mechanics of diseases like Alzheimer’s but also for inspiring the development of new treatment paradigms. The research conducted at institutions like Boston Children’s Hospital underscores the essential interplay between basic science and clinical applications. As strategies evolve, there is hope that we will soon see more effective treatments emerging from these discoveries, providing relief to millions suffering from neurodegenerative diseases.
The Impact of Federal Funding on Alzheimer’s Research
Federal funding plays a pivotal role in advancing Alzheimer’s research and facilitating breakthroughs that otherwise may not be possible. As Stevens mentioned, the initial phase of her research career was significantly supported by the National Institutes of Health (NIH), which provided the necessary resources to explore the fundamentals of microglial biology. This backing is essential for fostering innovative research that leads to significant medical advancements in understanding brain health.
Additionally, federal investments in Alzheimer’s research not only sustain individual labs but also stimulate collaborative networks that enhance scientific discoveries. As knowledge expands through these funded projects, the potential for impactful treatments increases, underscoring the critical need for continued support in the realm of neurodegenerative diseases. With the aging population and rising case numbers, the case for robust funding in Alzheimer’s research has never been more compelling.
Revolutionizing our Understanding of Synaptic Plasticity
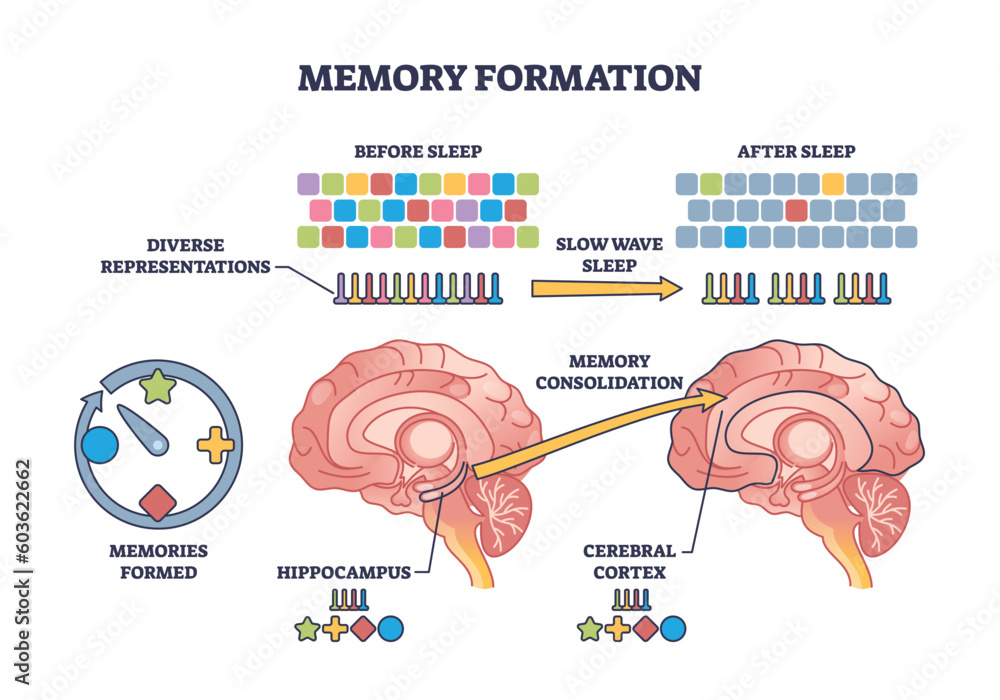
One of the most exciting dimensions of modern neuroscience is the profound discovery of synaptic plasticity and its implications for learning and memory. Stevens’ research underscores how microglial cells play an integral role in shaping synaptic connections within the brain during development and in response to injuries throughout life. This dynamic process illustrates how our brain continuously adapts, reconfiguring itself as it encounters new experiences.
The toppling of long-held beliefs about microglia’s traditional role opens new research avenues grounded in the idea that these cells contribute not just to protection but also to the promotion of cognitive processes. By understanding how disruptions in microglial function can lead to harmful plasticity in neurodegenerative diseases like Alzheimer’s, researchers can propose more effective interventions that could restore normal synaptic functions and combat cognitive decline.
Beth Stevens: A Pioneer in Neuroscience
Beth Stevens stands out as a transformative figure in neuroscience, especially in the context of Alzheimer’s research. Her pioneering work on microglial cells has fundamentally altered the understanding of how the brain’s immune system interacts with neuronal health. Stevens’ approach exemplifies how curiosity-driven research can lead to groundbreaking discoveries that have far-reaching implications for treating neurodegenerative diseases.
Further solidifying her impact, Stevens has earned recognition for her innovative contributions, including being awarded the MacArthur Fellowship, a testament to her influential work in the field. Her dedication inspires a new generation of researchers to explore the intricate relationships between brain immunity and disease, reinforcing the importance of basic science as a foundation for future therapeutic developments.
The Future of Alzheimer’s Biomarkers and Early Detection
The quest for effective Alzheimer’s treatment is intrinsically linked to the identification of reliable biomarkers. Recent advancements in research are aiming to uncover specific indicators that could signal the onset of Alzheimer’s disease before clinical symptoms arise. As highlighted in Stevens’ research, early detection is critical, as it provides opportunities for more effective interventions and management strategies, potentially altering disease trajectories.
Deploying innovative technologies and collaborative research efforts will be paramount in establishing these biomarkers. By studying the mechanisms behind microglial dysfunction and other cellular behaviors, researchers can develop screening tools that could revolutionize how Alzheimer’s is diagnosed and treated, ultimately enhancing the lives of millions of individuals at risk of neurodegenerative diseases.
Collaboration: The Key to Unlocking New Solutions
Collaboration across disciplines is fundamental to advancing the science of neurodegenerative diseases, including Alzheimer’s. The merging of fields such as genetics, immunology, and neurology fosters a holistic approach to understanding complexities that accompany diseases of the brain. Stevens’ collaboration with institutions and fellow scientists highlights how shared knowledge can lead to comprehensive strategies aimed at tackling the multifaceted challenges of Alzheimer’s.
These collaborative efforts enrich the research landscape, encouraging innovative thinking and enabling the exploration of novel therapeutic avenues. By leveraging diverse expertise and resources, researchers can construct a more nuanced understanding of Alzheimer’s, ultimately leading to the development of effective treatments that target its underlying causes and symptomatic progression.
The Societal Impact of Alzheimer’s Research and Treatment
The societal implications of Alzheimer’s research extend far beyond individual patients, affecting families, healthcare systems, and the economy as a whole. As the prevalence of Alzheimer’s continues to rise, the associated caregiver burden and healthcare costs escalate, demanding urgent responses from researchers and policymakers alike. Insights from Stevens’ work underscore the necessity for innovative approaches that not only seek to alleviate symptoms but also aim to fundamentally alter disease progression.
By championing breakthroughs in Alzheimer’s research, there is potential to dramatically shift the economic burden associated with this disease. Investments in early detection and effective treatment solutions can herald new standards of care that enhance not only patient lives but also alleviate pressures on healthcare resources, leading to lasting positive changes within communities and society at large.
Frequently Asked Questions
What is the role of microglial cells in Alzheimer’s research?
Microglial cells play a crucial role in Alzheimer’s research as they function as the brain’s immune system. They monitor for signs of illness or injury, remove dead or damaged cells, and prune synapses that transmit information between neurons. Recent studies show that improper pruning by microglia can contribute to neurodegenerative diseases, including Alzheimer’s, highlighting their importance in ongoing research.
How is Beth Stevens contributing to Alzheimer’s research?
Beth Stevens is significantly advancing Alzheimer’s research through her groundbreaking work on microglial cells and their role in the brain’s immune system. Her discoveries have identified how improper synaptic pruning by these immune cells can lead to Alzheimer’s and other neurodegenerative diseases, paving the way for new treatments and earlier detection methods.
What implications do microglial cells have for Alzheimer’s treatment?
Microglial cells have profound implications for Alzheimer’s treatment because they are central to the brain’s immune response and synaptic health. Understanding how microglial dysfunction contributes to Alzheimer’s disease could lead to innovative therapies that target these cells, offering new hope for those affected by neurodegenerative diseases.
How does understanding the brain’s immune system impact Alzheimer’s research?
Understanding the brain’s immune system, particularly through the study of microglial cells, is vital for Alzheimer’s research. It provides insights into how the immune response can affect synapse pruning, neuronal health, and the overall progression of neurodegenerative diseases, guiding the development of potential treatments and interventions.
What are the potential benefits of Beth Stevens’ research on Alzheimer’s?
Beth Stevens’ research on microglial cells in relation to Alzheimer’s could lead to the discovery of new biomarkers for early disease detection and innovative therapies. Her work aims to enhance our understanding of neurodegenerative diseases, potentially impacting millions of people living with Alzheimer’s and improving their quality of life.
Why are microglial cells considered a focus in neuroscience related to Alzheimer’s?
Microglial cells are a key focus in neuroscience related to Alzheimer’s due to their dual role in protecting the brain and their potential to cause harm through improper synaptic pruning. Research in this area is crucial as it uncovers how these immune cells can be targeted for developing new strategies to combat Alzheimer’s and other neurodegenerative diseases.
What impact does Alzheimer’s research have on the future of neurodegenerative disease treatments?
Alzheimer’s research, particularly studies focused on microglial cells and the brain’s immune system, is poised to significantly impact the future of neurodegenerative disease treatments. As researchers uncover the cellular and molecular mechanisms at play, it opens pathways for innovative therapies that could alter the course of diseases like Alzheimer’s, improving outcomes for patients.
How can curiosity-driven research aid in Alzheimer’s disease understanding?
Curiosity-driven research, like that conducted by Beth Stevens, is essential for advancing our understanding of Alzheimer’s disease. It allows scientists to explore fundamental questions about brain function and immune responses, leading to unexpected discoveries that can have profound implications for the development of new treatments and therapeutic approaches for neurodegenerative diseases.
| Key Point | Details |
|---|---|
| Focus of Research | Neuroscientist Beth Stevens investigates microglial cells, the brain’s immune system, to understand their role in Alzheimer’s and other neurodegenerative diseases. |
| Microglial Function | Microglia remove damaged cells and prune synapses to facilitate neuronal communication, but improper pruning can contribute to diseases. |
| Impact of Research | Stevens’ work has the potential to change the treatment landscape for about 7 million Americans suffering from Alzheimer’s. |
| Future Projections | The number of Alzheimer’s cases is expected to double by 2050, increasing care costs significantly. |
| Funding and Support | Stevens’ research has been supported by federal funding, primarily from the National Institutes of Health, allowing her to explore complex neurological questions. |
| Scientific Curiosity | Stevens emphasizes the importance of curiosity-driven research, which lays the groundwork for significant advancements in disease understanding and treatment. |
Summary
Alzheimer’s research is crucial in the fight against this devastating disease affecting millions of people. With the pioneering work of scientists like Beth Stevens, our understanding of the brain’s immune response has grown, shedding light on the mechanisms underlying Alzheimer’s and facilitating the development of potential therapies. As the population ages and the incidence of Alzheimer’s increases, continued investment in basic science and innovative research is essential for creating effective solutions that can improve the lives of those impacted by this condition.